
The Hidden Cardiac Crisis - COVID-19's Lasting Assault on Hearts Worldwide
The Hidden Cardiac Crisis: COVID-19's Lasting Assault on Hearts Worldwide
Advanced imaging reveals persistent heart damage in millions of recovered patients, reshaping cardiovascular medicine and creating unprecedented market opportunities
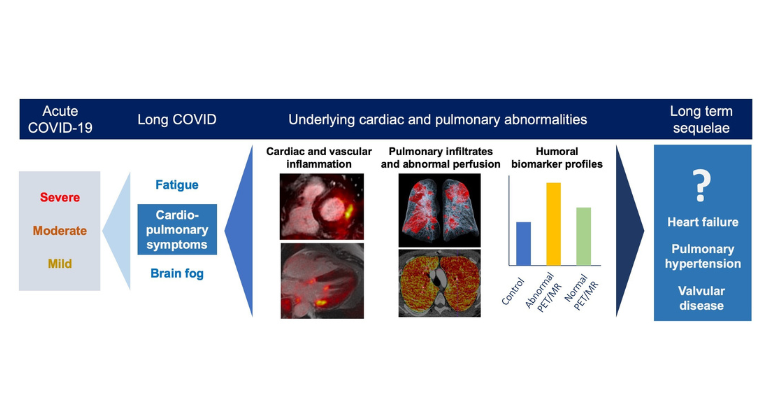
In the sterile corridors of Mount Sinai Hospital, Dr. Zahi Fayad's team made a discovery that would fundamentally alter our understanding of COVID-19's true toll. Using cutting-edge PET/MRI technology to peer inside the hearts of 191 recovered patients, they found something deeply unsettling: metabolically active inflammation persisting up to a year after infection, even when conventional tests showed normal results.
This revelation represents just the tip of an iceberg that medical researchers worldwide are now scrambling to understand. Five years after the pandemic began, a growing body of evidence reveals that SARS-CoV-2 has left an indelible mark on the cardiovascular systems of millions, creating what amounts to a new chronic disease cohort the size of the global hypertension population.
When Hearts Remember What Bodies Forget
The Mount Sinai study, the largest of its kind using hybrid PET/MRI imaging, represents a watershed moment in post-COVID research. Unlike traditional echocardiograms or basic blood tests that often return normal readings, this advanced technology revealed persistent inflammation in both heart and lung tissue that standard medical assessments completely missed.
The implications are staggering. Patients walking around with apparently clean bills of health are harboring inflammatory processes that may predispose them to future heart failure, valvular disease, and pulmonary hypertension. The inflammation appears to be metabolically active, suggesting ongoing tissue damage rather than merely residual scarring.
This discovery aligns with equally troubling findings from cardiac magnetic resonance imaging studies. Research published in 2024 examined 54 recovered COVID-19 patients using detailed cardiac MRI protocols. The results were sobering: 29 patients—over half—showed positive findings for myocarditis. Most had experienced only mild COVID-19 symptoms, demolishing the assumption that severe acute illness was necessary for lasting cardiac damage.
Among those with MRI evidence of heart inflammation, the damage was extensive. Nearly one-third exhibited myocardial edema, indicating active swelling of heart muscle. Twenty percent showed impaired left ventricular function, while ten percent had compromised right heart function. These are not subtle abnormalities detectable only by sophisticated equipment—they represent meaningful reductions in the heart's ability to pump blood effectively.
The Arithmetic of Cardiac Devastation
A comprehensive 2025 systematic review analyzing multiple studies has revealed the true scope of COVID-19's cardiovascular assault. The numbers paint a picture of widespread, persistent dysfunction affecting millions globally.
Left ventricular strain—a sensitive measure of heart muscle function—remained impaired in 34% of patients seven months after infection. This finding carries particular weight because reduced strain measurements correlate directly with increased risk of major adverse cardiac events, including heart attack and sudden death. In practical terms, more than one in three COVID survivors harbor subtle but measurable heart dysfunction that elevates their risk of future cardiovascular catastrophe.
The persistence of these abnormalities defies medical expectations. In one study tracking 229 patients over time, left ventricular strain remained reduced in 36% at five months, with right heart strain affected in an additional 7.2%. Most concerning, follow-up at twelve months showed no improvement in subclinical myocardial dysfunction, suggesting that whatever damage COVID-19 inflicts on heart muscle may be permanent.
Cardiac MRI abnormalities follow a similar pattern of stubborn persistence. At six months post-infection, one in five patients showed ongoing abnormalities on advanced cardiac imaging. At twelve months, three out of five who had abnormalities at six months continued to show persistent changes. The heart, it appears, has a long memory for COVID-19's assault.
Scars That Tell Stories
The structural changes COVID-19 leaves behind read like a pathologist's catalog of cardiac injury. Late gadolinium enhancement—the MRI signature of heart muscle scarring—appears in 54% of recovered patients. This scarring follows two distinct patterns, each telling its own story of viral damage.
Twenty-six percent of patients show myocarditis-like scarring, the kind typically seen after viral infections of the heart muscle. But equally troubling, 22% exhibit infarction and ischemia patterns—the type of scarring usually associated with heart attacks caused by blocked coronary arteries. Among patients showing these ischemic patterns, two-thirds had no previous history of coronary artery disease, strongly suggesting that COVID-19 directly caused this damage.
The presence of myocardial edema—heart muscle swelling—in 54% of patients provides additional evidence of ongoing injury and inflammation. This finding, combined with the scarring patterns, paints a picture of a virus that attacks the heart through multiple mechanisms, leaving behind a complex landscape of damage that standard medical approaches struggle to detect and treat.
The Democracy of Viral Damage
One of the most unsettling aspects of COVID-19's cardiac effects is their democratic nature. While patients with severe acute illness face higher risks, even mild infections can result in measurable and persistent heart damage. This finding has profound implications for the hundreds of millions who experienced seemingly minor COVID-19 symptoms and assumed they escaped unscathed.
The data reveals a clear severity gradient—hospitalized patients show higher frequencies of scarring and edema compared to those with mild disease. However, the absolute numbers affected across all severity levels means that the majority of COVID-19's cardiac victims experienced only mild acute symptoms. They represent a vast, largely unrecognized population harboring subclinical heart disease.
Recent research has identified genetic factors that influence susceptibility to these long-term effects. Individuals with non-O blood types face 26% higher rates of post-COVID cardiovascular events, representing one of the first documented examples of gene-pathogen interaction increasing heart disease risk. This finding adds another layer of complexity to risk stratification and suggests that personalized approaches to post-COVID care may be necessary.
A Global Health Transformation
The scale of COVID-19's cardiovascular impact becomes clear when viewed through the lens of population health. A 2025 meta-analysis examining nearly three million patients across 37 studies found that 15% of all COVID-19 patients develop cardiovascular complications. Applied to the estimated one billion people worldwide who have contracted COVID-19, this translates to approximately 150 million individuals now living with virus-induced heart problems.
The specific complications reveal the breadth of COVID-19's cardiac assault. Heart failure affects 14% of patients, while arrhythmias occur in 16%. Acute myocardial infarction—heart attack—strikes 21% of COVID patients. Most alarming, cardiomyopathy—disease of the heart muscle itself—affects fully one-third of patients, making it the most common cardiovascular sequel of COVID-19 infection.
Even patients who avoided hospitalization face elevated risks. Those with mild COVID-19 show a 52% higher chance of stroke and 72% higher risk of heart failure compared to uninfected individuals. These risks persist for up to three years after infection, fundamentally altering the cardiovascular risk profile of hundreds of millions of people worldwide.
The Long Shadow of Infection
The duration of COVID-19's cardiovascular effects has proven far longer than initially anticipated. Multiple 2024 studies demonstrate that the virus doubles the risk of heart attack, stroke, and death for up to three years following infection. For hospitalized patients, this risk elevation is four-fold, comparable to the cardiovascular risk associated with Type 2 diabetes.
This persistent risk elevation follows a clear pattern across time. The elevated risk remains statistically significant within each of the three follow-up years, showing no signs of declining back to baseline. For many patients, COVID-19 infection represents a permanent upward shift in their cardiovascular risk profile, similar to developing a chronic disease like diabetes or hypertension.
The heart failure risk deserves particular attention. COVID-19 recovery subjects face an additional 90% risk of developing heart failure within nine months of acute infection. Given that heart failure affects millions globally and carries a five-year mortality rate worse than many cancers, this finding represents a public health crisis of unprecedented scale.
Investment Implications and Market Transformation
For professional investors and traders, COVID-19's cardiovascular legacy represents a fundamental shift in healthcare demand patterns. The creation of a 150-million-person cohort requiring ongoing cardiac monitoring and treatment has profound implications across multiple sectors.
The advanced imaging market stands to benefit most immediately. The need for sophisticated PET/MRI scans, cardiac MRI studies, and specialized inflammation tracers creates sustained demand divorced from traditional economic cycles. Companies like Siemens Healthineers, with their comprehensive cardiac imaging portfolios, are positioned to capture significant market share in what amounts to a new, medically necessary service category.
Remote cardiac monitoring represents another clear winner. The need to track subclinical dysfunction in millions of patients creates unprecedented demand for wearable devices, mobile cardiac telemetry, and AI-powered analysis platforms. Companies like iRhythm Technologies, which specialize in ambulatory cardiac monitoring, face a dramatically expanded addressable market.
The pharmaceutical implications are equally significant. The high incidence of heart failure, arrhythmias, and cardiomyopathy creates sustained demand for cardioprotective medications, heart failure drugs, and anti-arrhythmic therapies. The market represents a multi-decade revenue opportunity that transcends typical patent cycles and drug development timelines.
The Actuarial Reckoning
Perhaps most significantly for institutional investors, COVID-19's cardiovascular effects represent a fundamental challenge to actuarial assumptions underlying life insurance, health insurance, and pension obligations. The discovery that infection creates persistent elevation in cardiovascular risk for at least three years—and potentially longer—requires wholesale revision of mortality and morbidity projections.
Health insurers face a particularly acute challenge. The 15% rate of cardiovascular complications among COVID patients translates to millions of individuals requiring ongoing cardiac care, advanced imaging, and expensive medications. This burden will flow through to medical loss ratios over the coming years, potentially requiring significant premium adjustments.
Life insurers must grapple with the implications of shortened life expectancy among COVID survivors, particularly those with non-O blood types who face elevated risks. The industry's reliance on historical mortality tables may prove inadequate for pricing policies in a post-COVID world.
The Path Forward
As the medical community grapples with COVID-19's cardiovascular legacy, several trends are emerging that will shape both clinical practice and investment opportunities. The shift toward advanced cardiac imaging as a standard component of post-COVID care creates sustainable demand for high-margin diagnostic services. The recognition that mild COVID-19 can cause significant heart damage expands the pool of patients requiring ongoing monitoring far beyond those who were hospitalized.
The development of targeted therapies for post-COVID cardiovascular complications represents a nascent but potentially lucrative pharmaceutical opportunity. Companies developing anti-inflammatory agents, anti-fibrotic drugs, and specialized heart failure medications for post-COVID patients could capture significant market share in what amounts to a new disease category.
The evidence is now overwhelming: COVID-19 has created a global population of cardiac patients whose needs will strain healthcare systems and create investment opportunities for decades to come. The virus that began as a respiratory illness has revealed itself to be a cardiovascular disease of unprecedented scale, one whose full impact is only now becoming clear.
For professional traders and institutional investors, the message is unambiguous: COVID-19's cardiovascular legacy represents a fundamental shift in healthcare demand that transcends traditional market cycles. The companies positioned to serve this new patient population—whether through advanced diagnostics, remote monitoring, or targeted therapeutics—stand to benefit from a multi-decade growth opportunity born from one of the most significant public health crises in modern history.